A Guide to Clinical Differential Diagnosis of Oral Mucosal Lesions
Course Number: 110
Course Contents
Reactive Soft Tissue Enlargements
Reactive soft tissue enlargements are caused by injury, such as infections, physical trauma, chemical trauma, or allergic reactions. Reactive soft tissue enlargements usually have a rapid onset (short duration) and may increase and decrease (fluctuate) in size and usually eventually regress. Reactive enlargements are often, but not always, tender or painful and usually have a more rapid growth rate (measured in hours to weeks) than tumors. Sometimes patients with reactive enlargements will be able to report the source of injury. Sometimes reactive lesions are associated with tender lymph nodes and systemic manifestations, such as fever and malaise. Once it is decided that a soft tissue enlargement is reactive, the next step is to determine what the lesion is reacting to, such as bacterial, viral, or fungal infections or chemical or physical injury.
Some examples of reactive soft tissue enlargements:
Mucocele (salivary extravasation phenomenon)
Necrotizing sialometaplasia
Periodontal abscess
Radicular (periapical) abscess
Fibrous hyperplasia
Inflammatory papillary hyperplasia
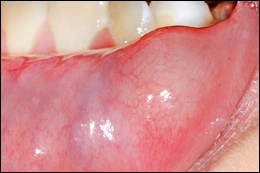
Salivary extravasation phenomenon, usually called a "mucocele" occurs when a salivary gland duct is ruptured and mucus forms a pool in the surrounding connective tissue. It most commonly occurs in locations that are easily traumatized, such as the lower lip. Clinical features include a well localized, compressible or fluctuant soft tissue enlargement. The patient may report that the lesion increases and decreases (fluctuates) in size. The surface of the lesion may be blue to purple or normal in color. Sometimes these lesions resolve spontaneously. Persistent lesions should be excised to minimize recurrence. Lesions must be examined microscopically to exclude salivary gland tumors.
Mucocele
Necrotizing sialometaplasia is a reactive lesion of salivary gland origin. The cause is local ischemia producing infarction of salivary acini. The ensuing inflammation causes squamous metaplasia of ducts and hyperplasia of the surface stratified squamous epithelium. The vast majority of cases occur on the posterior lateral hard palate. The lesion begins acutely with swelling and pain or numbness. Eventually an ulcer forms within the enlargement. Necrotizing sialometaplasia resembles squamous cell carcinoma and/or mucoepidermoid carcinoma clinically and microscopically. Treatment is incisional biopsy and microscopic diagnosis. No further treatment is necessary once the diagnosis is established, as the lesion resolves spontaneously in weeks to several months.
Necrotizing sialometaplasia
Periodontal abscess is an accumulation of pus within a periodontal pocket. It may be associated with pain, tenderness to palpation of the gingiva, tooth mobility, and erythema of the overlying gingiva. Radiographs may reveal loss of alveolar bone. Probing the pocket often allows release of purulent material. Tender lymphadenopathy may accompany a periodontal abscess. Treatment consists of draining the purulent material and debriding the pocket. The presence of fever and malaise indicates a systemic infection, and the patient should be placed on antibiotics. Follow-up periodontal therapy is necessary.
Periodontal abscess
Periapical abscess is an accumulation of purulent material in the periapical region of a tooth with a necrotic pulp. The involved tooth may or may not be symptomatic. As a periapical abscess becomes larger it can perforate the cortical bone, accumulate in the connective tissue, and form a compressible, painful soft tissue enlargement. Sometimes the purulent material perforates the overlying oral epithelium and forms a channel (sinus track) through which the material may drain into the oral cavity. Parulis (“gumboil”) is the soft tissue enlargement resulting from the accumulation of acute and chronic inflammation and granulation tissue at the opening of the sinus track onto the oral mucosa. Treatment of periapical abscess involves treatment of the involved tooth by root canal therapy or extraction.
Periapical abscess leading to parulis
Inflammatory papillary hyperplasia represents an overgrowth of epithelial and fibrous connective tissue, usually as a response to chronic irritation from a denture. The lesion occurs on the hard palate or mandibular alveolar mucosa underneath a denture. The surface of the lesion is bumpy, nodular, or velvety, and often erythematous. The patient may complain of pain or burning in association with the lesion, or the lesion may be asymptomatic. Lesions often have concomitant overgrowth of candidal organisms. The patient should remove the denture as much as possible, and the lesion should be reevaluated. If the papillary overgrowth is minimal, the lesion does not need to be removed. More extensive lesions should be excised. The denture should be remade and the patient educated about removing the denture at night and cleaning the denture. If candidosis is present it should be treated with a topical antifungal ointment or cream applied to the inner surface of the denture.
Inflammatory papillary hyperplasia
To view the Decision Tree for Oral Mucosal Lesions, click on one of the options shown.
To view the Decision Tree for Oral Mucosal Lesions, click on one of the options shown.







 View Interactive
View Interactive View as PDF
View as PDF View as GIF
View as GIF